We’re thrilled to invite all UAMS-affiliated faculty and staff to join us for two inspiring days celebrating innovation in translational research!
Location: Winthrop P. Rockefeller Cancer Institute Conference Center, 10th floor.
The themes for this year’s expanded TRI Research Day are:
Day 1: Integrating Data to Further Translational Science
Day 2: Community Health Impact Day: Advancing Health through Translational Research
- Dynamic keynote speakers
- Oral presentations from TRI-supported investigators
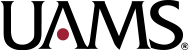
- A poster session highlighting research from TRI’s funding and training programs
- Community-engaged programming
- Great opportunities for networking!
Meet Our Keynote Speakers:

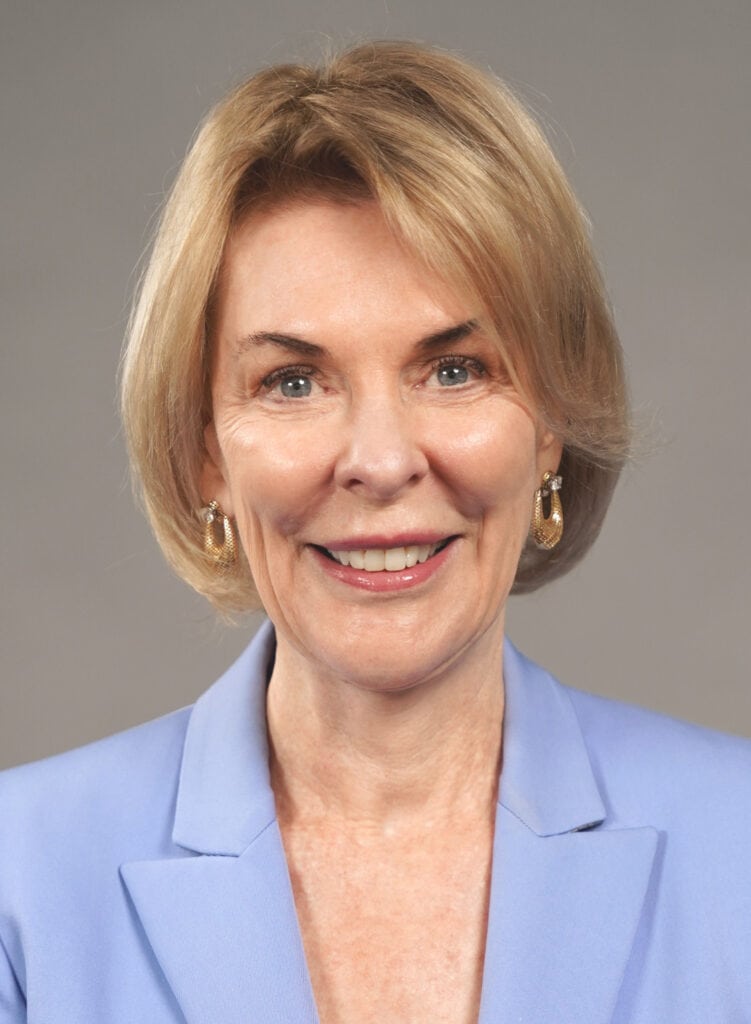
- Elizabeth A. Shenkman, Ph.D., University of Florida
Presentation: Translating Discoveries to Practice Using Real World Data and Clinical Settings - Sharla Smith, Ph.D., MPH, University of Kansas Medical Center
Presentation: Achieving Birth Equity: Addressing Systemic Barriers in Black Maternal Health
Register now to save your spot.
We can’t wait to see you there!
Contact: Christi Madden, cmadden2@uams.edu.